Select Health Medicare
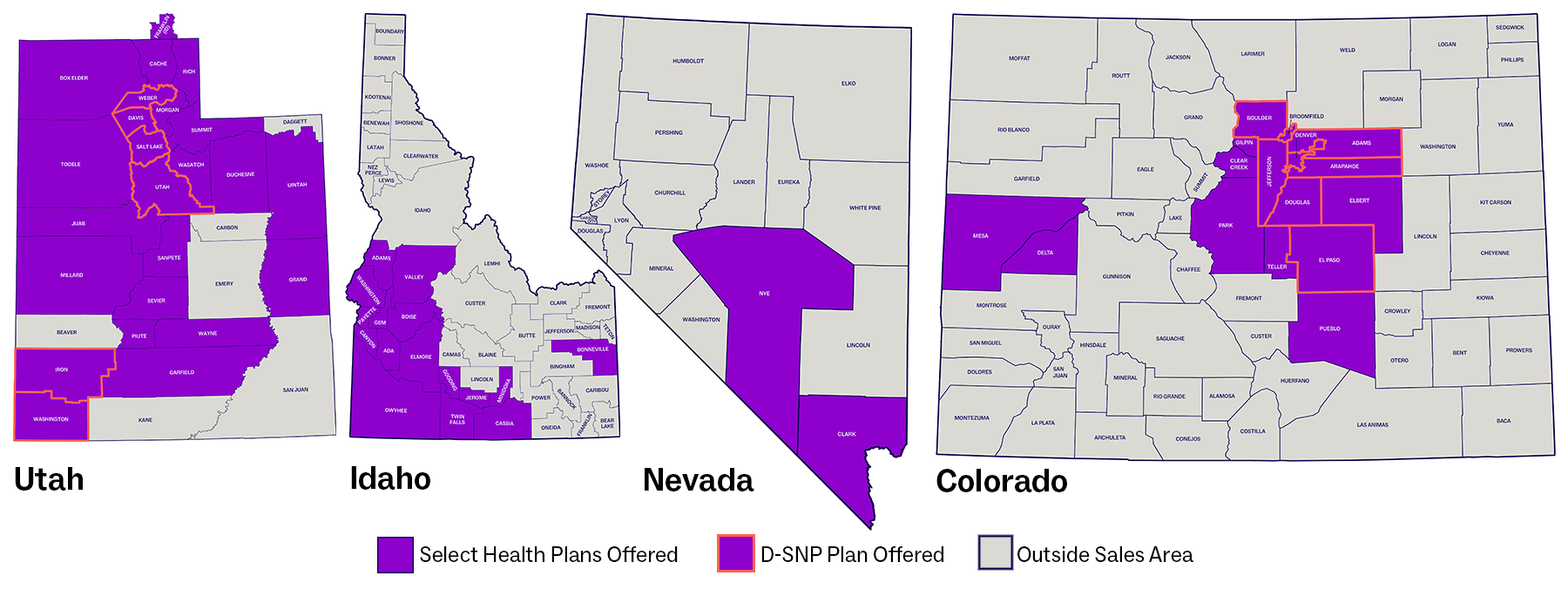
Select Health Medicare plans for Medicare Advantage beneficiaries are available to residents in Utah, Idaho, Nevada, and Colorado based on the coverage maps below.
Physicians and other healthcare professionals who participate on Select Health Medicare agree to comply with the standards and regulations set forth by the Centers for Medicare & Medicaid Services (CMS). These standards address preauthorization, balance billing, requests needing documentation, general compliance and fraud/waste/abuse, regulations and guidance, Medicare Advantage marketing by providers, and STAR ratings.